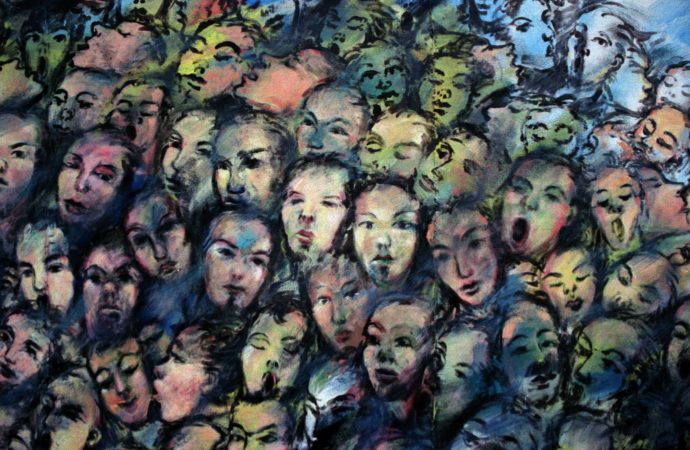
Dealing with psychotic patients takes more than looking at their diagnostic labels.
A psychosis occurs when someone loses contact with reality, usually due to hallucinations (feeling compelled to obey voices, for instance), or delusions (such as feeling persecuted). Ultimately, psychosis affects both the most basic routines, such as cooking a simple meal, and the most complex aspects of one’s personality, leading to destructive behavior or to a sense of isolation and depression.
Psychosis occurs rather frequently. According to a study from 2007, more than 3% of US citizens have a psychotic disorder. Thus, the severity of the problem should not be overlooked and focusing on the patients’ symptoms might be the crucial step to a better understanding of the disease.
During the 60s, Kurt Schneider identified certain typical symptoms in schizophrenic patients, such as delusional perceptions or thoughts withdrawal (the perception that one’s own thoughts are being taken away from their brains). He coined them as First Rank Symptoms (FRS) and regarded them as diagnostic tools, since when any of these symptoms were present, the patient could be diagnosed as schizophrenic.
Dr Henriette Heering, whose PhD-project focus on the heterogeneity of psychotic patients, argues that these symptoms ‘should no longer be considered exclusive of schizophrenia’, since they are also present, for instance, in psychotic patients suffering from self-disturbance (a disturbed perception of the self). In this interview, she explains why it is crucial to look at patients’ symptoms to understand their heterogeneity.
What are the most commonly observed symptoms in psychotic patients?
First of all, psychotic disorders comprise a wide range of disorders, being schizophrenia the most severe one. The so-called ‘fever of schizophrenia’ causes psychotic patients to suffer the most serious symptoms. Nevertheless, these severe symptoms can also be caused by drug abuse, for instance. (view table below for an overview of the symptoms commonly described by psychotic patients.).

What is the major difference between Negative Symptoms and (FRDs), regarding the social behavior of psychotic patients?
Negative Symptoms are a cluster of symptoms associated with lack of motivation or enjoyment. People who lack these feelings have a hard time to create and maintain a social life. First Rank Delusions, on the other hand, have a different kind of influence on social functioning, namely they influence the interaction between the self and the other.
Why are Symptom Clusters so important in studying psychotic disorders?
Symptom Clusters show how different symptoms, within the same diagnosis, are connected. For instance, imagine that tea cans represent schizophrenic patients. If I only analyze their lids, I conclude they are all square-shaped and hence the same. However, if I open the tea cans, I see they all have a different content (which represents experience of illness). In other words, to gain more insight into psychotic disorders, symptom clusters are more important than diagnoses.
What triggered you to investigate the heterogeneity and self-disturbance of psychotic disorders?
Giving behavioral therapy to people with psychotic disorders made me realize that, even though they all had the same diagnosis, they were very different with respect to their symptoms, quality of life and social functioning.
Another interesting aspect was that many patients complained about self-disturbance, which affected their sense of identity or involvement in conversations. So, talking to different patients was the starting point for my interest in their heterogeneity and self-disturbance.
The GROUP and the SELF
What is the Genetic Risk and Outcome Psychosis (G.R.O.U.P.)? And how did it help your research?
Basically, the G.R.O.U.P. research provided most of my results. It is a big naturalistic follow-up study about psychosis in the Netherlands. Patients, their siblings and parents, and healthy controls are followed over six years, and data is measured every three years, which allows a great insight into the disease development (see figures below).
Why did you decide to create the SELF (Self-Experience Lifetime Frequency Scale) questionnaire?
The SELF is based on the current psychotic disorders’ diagnostic tools, but allow us to quickly address both the prevalence and severity of twelve symptoms in large amounts of volunteers. This was just too complicated with the current existent questionnaires. With the SELF, we are able to diagnose whether somebody suffers from self-disturbance, but the SELF cannot be used to classify the self-disturbance.
What future research do you suggest?
I would like to compare the different existent tests and determine which one is the best to classify self-disturbance. In addition, since other studies show that people with self-disturbance process information differently, I would like to investigate whether this influences patients’ social behavior.
 Henriëtte (also known as Jet) is a vivid and people-oriented person. She successfully defended her thesis ‘On heterogeneity and self-disturbance in psychotic disorders’. After her masters in clinical psychology, she became a diagnostic specialist at Jellinek youth clinic, where she performed psychological tests in patients. In 2011, she joined the Genetic Risk and Outcome Psychosis (G.R.O.U.P.) and started her PhD-project, which was led by Lieuwe de Haan.
Henriëtte (also known as Jet) is a vivid and people-oriented person. She successfully defended her thesis ‘On heterogeneity and self-disturbance in psychotic disorders’. After her masters in clinical psychology, she became a diagnostic specialist at Jellinek youth clinic, where she performed psychological tests in patients. In 2011, she joined the Genetic Risk and Outcome Psychosis (G.R.O.U.P.) and started her PhD-project, which was led by Lieuwe de Haan.References:
Heering, H., van Haren, N., & Derks, E. (2013). A two-factor structure of first rank symptoms in patients with a psychotic disorder Schizophrenia Research, 147 (2-3), 269-274 DOI: 10.1016/j.schres.2013.04.032
Heering, H., Koevoets, G., Koenders, L., Machielsen, M., Meijer, C., Kubota, M., de Nijs, J., Cahn, W., Hulshoff Pol, H., de Haan, L., Kahn, R., & van Haren, N. (2015). Structural MRI Differences between Patients with and without First Rank Symptoms: A Delusion? Frontiers in Psychiatry, 6 DOI: 10.3389/fpsyt.2015.00107
Nelson B, Whitford TJ, Lavoie S, & Sass LA (2014). What are the neurocognitive correlates of basic self-disturbance in schizophrenia? Integrating phenomenology and neurocognition: Part 2 (aberrant salience). Schizophrenia research, 152 (1), 20-7 PMID: 23863772
Perälä, J., Suvisaari, J., Saarni, S., Kuoppasalmi, K., Isometsä, E., Pirkola, S., Partonen, T., Tuulio-Henriksson, A., Hintikka, J., Kieseppä, T., Härkänen, T., Koskinen, S., & Lönnqvist, J. (2007). Lifetime Prevalence of Psychotic and Bipolar I Disorders in a General Population Archives of General Psychiatry, 64 (1) DOI: 10.1001/archpsyc.64.1.19
Heering H.D., Janssens M., Boyette L-L., Van Haren N.E.M., Lataster T. and GROUP Investigators (Submitted for publication). Persistance of symptoms associated with functional outcome in non-affective psychotic disorders: a longitudinal study.
Heering H.D., Van Haren N.E.M., Meijer C.J., Myin-Germeys I., Van Os J. and De Haan L. (Submitted for publication). Social functioning in patients with a psychotic disorders.
Heering H.D., Goedhart S. and GROUP Investigators (Submitted for publication). Disturbed experience of self: psychometric analysis of the SELF Experience Lifetime Frequency scale (SELF).
Picture: https://www.researchgate.net/profile/Henriette_Heering<